A recent study conducted by researchers in China has revealed that specific immune cell types are dysregulated in individuals suffering from primary Sjögren’s disease. The alterations identified may play a significant role in the progression of the condition and its severity.
“Our study demonstrates significant alterations in circulating immune cell populations in patients with [primary Sjögren’s], linking these changes to clinical disease activity,” the researchers stated.
The team emphasized three immune cell types that could serve as biomarkers for the disease and potential targets for future therapeutic approaches. “These findings may provide mechanistic insights into … pathogenesis [disease development] and establish a foundation for developing … targeted therapeutic strategies,” the scientists added.
Published in the International Journal of Rheumatic Diseases, their study titled “Immunophenotypic Profiling Reveals Circulating Lymphocyte Dysregulation in Primary Sjögren’s Syndrome” explores the complexities of this autoimmune condition, which arises when the immune system mistakenly attacks the body’s own cells, predominantly affecting tear and salivary glands. This often leads to the hallmark symptoms of dry eyes and dry mouth.
When the syndrome occurs independently, it is classified as primary Sjögren’s. Various immune cell types, particularly B cells and T cells, are believed to contribute to the disease. B cells are known for producing antibodies, while T cells help coordinate the immune response and eliminate infected or abnormal cells.
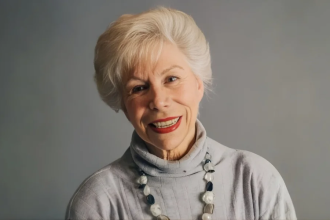
In their investigation, the researchers analyzed blood samples from 43 individuals with primary Sjögren’s—averaging 43.5 years of age, with approximately 95% being female—comparing them to a control group of 46 participants without chronic inflammatory disorders but matched in age and sex.
The findings indicated that B-cell levels were significantly elevated in the Sjögren’s cohort compared to controls, particularly highlighting an increase in CD21-/low B cells, which are also prevalent in other chronic immune conditions. The researchers found that higher levels of CD21-/low B cells correlated with greater disease severity in this group.
While certain immune changes typically manifest in specific tissues, dysregulation across circulating lymphocytes impacts the entire body. However, the study noted that “the relationship between peripheral immune cell alterations and clinical outcomes is not fully understood.”
The research demonstrated profound changes in peripheral lymphocyte subsets among Sjögren’s patients, revealing distinctive dysregulation patterns among T and B cell populations. Some B-cell subtypes exhibited significantly increased levels, while others were notably lower, with specific levels correlating to disease severity according to the EULAR Sjögren’s Syndrome Disease Activity Index (ESSAI).
For T-cell subtypes, overall levels of T-helper (Th) and T-follicular helper (Tfh) cells did not differ significantly between groups, but the Sjögren’s patients exhibited notable variations. Increased levels of Th2 and Th17 cells, which are instrumental in coordinating immune responses, were reported, indicating their role in B cell hyperactivity and glandular inflammation, thereby contributing to the early stages of disease progression.
Additionally, the total cytotoxic T (Tc) cells were significantly elevated in those with Sjögren’s, showing a correlation with more severe disease severity based on ESSAI scores. The researchers also noted diminished levels of Tc1 and Tc17 subtypes in patients, suggesting that higher Tc1 counts might be associated with milder forms of the disease.
The identification of these cell types as potential mediators of disease activity highlights avenues for further investigation. According to the researchers, “The identification of CD21−/low B cells as potential mediators of disease activity, alongside Th17 or Tc cell imbalances, highlights actionable pathways for further exploration.”
While the findings offer a foundation for understanding immune dysregulation in primary Sjögren’s, the researchers advocate for future multicenter studies involving larger cohorts to validate these observations and assess their therapeutic implications. They acknowledged limitations in the study, noting that the disease population examined predominantly comprised individuals with milder forms of Sjögren’s, suggesting that those with more severe manifestations may exhibit different immune dysregulation patterns.